Avoid These 3 Common Insulin Injection Mistakes
Why Injection Technique Matters + Outline of This Guide
Insulin does the heavy lifting, but the way it gets under your skin decides how smoothly it works. Technique errors are widespread—studies in diabetes clinics routinely find large shares of users with at least one preventable mistake, from injecting in the same spot to pulling the needle out too quickly. The result can be more glucose variability, unexplained highs or lows, bruising, and a creeping sense that you’re “doing everything right” while numbers refuse to play along. The good news is that small, practical changes often deliver steadier results without changing your prescribed dose. Think of technique as the road surface under your tires: even a powerful engine rides better on a well‑paved street.
In this article, we’ll keep things simple, evidence‑informed, and immediately usable. You’ll see where common pitfalls happen, why they matter physiologically, and how to fix them with steps you can revisit at any time. While this guide offers general education, your personal plan should follow the advice of your healthcare team.
Outline at a glance:
– Mistake 1: Poor site rotation and needle reuse leading to lipohypertrophy and erratic absorption
– Mistake 2: Faulty injection technique (angle, needle length, skinfold use, priming/mixing, and hold time)
– Mistake 3: Mismanaging timing and temperature (meal timing, stacking, storage, and travel)
– Wrap‑up: A practical checklist you can print or save for easy reference
Why these three? Because they combine frequency with meaningful impact. For example, lipohypertrophy—those rubbery, raised patches created by repeated injections—appears in a sizable portion of insulin users in clinic audits and is directly linked with unpredictable absorption. Temperature extremes degrade insulin structure, making potency less reliable. And timing missteps, such as dosing too close to or too far from a meal, can skew post‑meal readings for hours. Addressing these three areas often produces a clearer pattern on your glucose meter or continuous monitor, reduces frustration, and supports safer adjustments with your clinician’s guidance. Keep reading with your routine in mind; you may spot one small change that pays off all week.
Mistake 1: Poor Site Rotation and Needle Reuse
Where you inject shapes how insulin absorbs. Repeatedly using the same small area—especially the abdomen near the navel—invites lipohypertrophy, those firm, sometimes lumpy regions beneath the skin. In these altered patches, insulin can absorb too slowly one day, too quickly the next, or hardly at all, resulting in higher variability and more corrections. Clinical surveys across diabetes centers report many users developing lipohypertrophy, and the risk climbs with years on insulin, frequent reuse of needles, and limited site rotation.
Rotation made practical: imagine a grid drawn over each approved site (abdomen, outer thighs, upper outer arms, upper buttocks/hips). Use an area about the size of your palm per week, moving methodically clockwise or in rows, and step at least a finger’s width away from your last injection. Simple habits help:
– Switch sides daily or weekly to distribute wear.
– Keep a rotation card or phone note to avoid guesswork.
– Skip bruised, scarred, or hardened spots until they recover.
Needle reuse is tempting for convenience or to “save” supplies, but it quietly raises problems. A needle’s tip degrades after a single use—microscopic barbs and bending increase tissue trauma, pain, and bleeding. Reused needles can also promote lipohypertrophy and raise the chance of partial dose delivery if the pathway clogs. Using a fresh needle for each injection supports smoother skin entries and more consistent absorption. If access or cost pressures influence reuse, discuss options with your care team or pharmacist; there may be programs or supply adjustments that reduce the burden without compromising safety.
Check your sites monthly. With clean hands, gently press and glide over common locations; note any rubbery or thickened patches. If you find them, rest those areas for several weeks while rotating elsewhere. Many people notice fewer unexplained highs after avoiding overused zones. In short: rotate like a methodical gardener tending different plots each season, and retire every needle after its single job is done. This duo—site rotation plus single‑use needles—often brings the first quick win in making readings steadier.
Mistake 2: Faulty Injection Technique (Angle, Depth, Priming, Mixing, Hold Time)
Even with perfect rotation, technique details can make or break dose accuracy. Start with needle length and angle. Modern short pen needles (for example, in the 4–6 mm range) generally reach the subcutaneous layer at a 90‑degree angle in most body types, lowering the chance of intramuscular injections that can cause rapid, unpredictable absorption and post‑dose lows. With longer needles or very lean areas, a lifted skinfold (pinch) and/or a 45‑degree angle can keep insulin in the intended layer. A simple rule of thumb: if you’re slim or using longer needles, pinch; if you use short needles and have average subcutaneous tissue, a relaxed, 90‑degree approach often works well.
Before injecting with a pen, prime to ensure the device is delivering reliably. Expel a small amount of insulin (as directed in your device’s instructions) to clear air from the needle and confirm a steady stream. Skipping priming can lead to partial doses—especially with new needles—creating highs that look mysterious on the surface. If you use a cloudy insulin (such as NPH or certain premixed types), gently roll the pen between your palms and invert it repeatedly until the suspension looks uniformly milky. Uneven mixing means variable potency from one injection to the next, a recipe for unpredictable results.
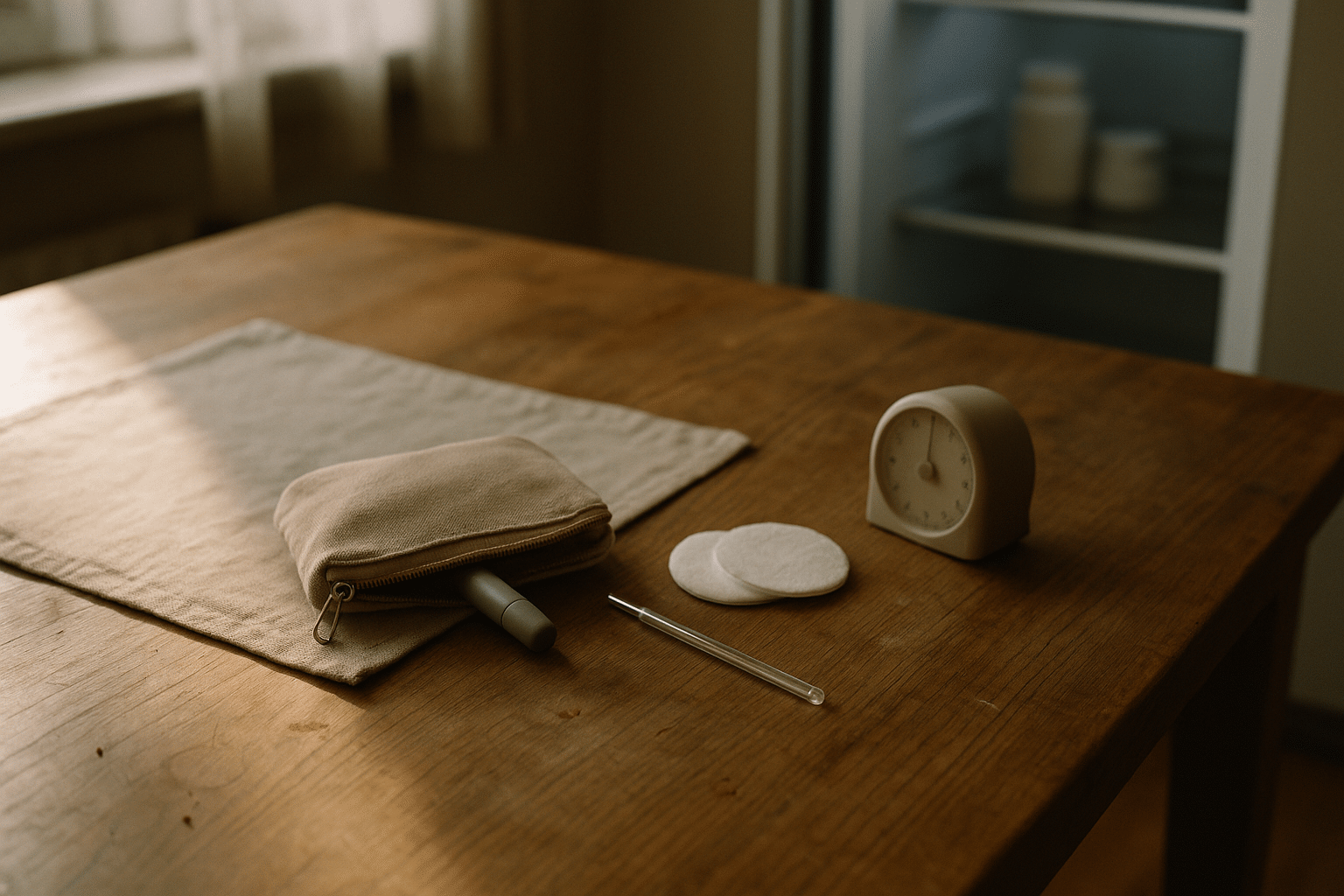
During the injection, insert the needle smoothly, depress the plunger fully, and keep the needle under the skin for a brief count before withdrawing. Holding for about 10 seconds after the plunger is fully down helps prevent back‑leakage, especially at higher doses. If you notice droplets at the skin or on the needle, lengthen that hold time slightly and avoid pressing too hard on the site afterward. Additional pointers:
– Let alcohol dry completely if you swab; wet skin can sting and pull insulin outward.
– Avoid injecting through clothing; fabric fibers can contaminate the needle and alter depth.
– Keep hands relaxed; tension can make insertion jerky and uncomfortable.
Finally, aim for consistency. Choose a comfortable posture and a stable, flat surface if you prepare doses at a table. Visual cues—like a small kitchen timer to pace your hold time, or a phone reminder to prime and mix when needed—turn “I think I did it” into a repeatable ritual. These details aren’t fussy; they’re the small hinges that swing big doors, translating prescribed units into predictable action.
Mistake 3: Mismanaging Timing and Temperature (Meals, Stacking, Storage, and Travel)
Insulin’s job is to meet glucose at the right place and time. Dose too early and you risk a dip before food arrives; too late, and post‑meal spikes surge before the insulin peaks. With rapid‑acting analogs, many clinicians suggest dosing shortly before eating—often within the 0–15 minute window—so onset aligns with meal absorption. With older human regular insulin, a longer lead time is commonly used because onset is slower. Your exact timing depends on your insulin type, your digestion, and the meal’s composition. High‑fat or high‑protein meals, for example, can delay glucose rise, sometimes calling for different strategies discussed with your care team.
“Stacking” corrections—taking extra doses before the previous one has peaked or cleared—can cause late‑onset lows. Know your insulin’s action profile (onset, peak, and duration) and give it time to work unless your plan specifies otherwise. A quick check before adding a correction: how long has it been since the last dose, where is your trend heading, and are other factors (exercise, alcohol, stress, illness) in play? A measured, plan‑based approach saves you from the rollercoaster of over‑correcting both ways.
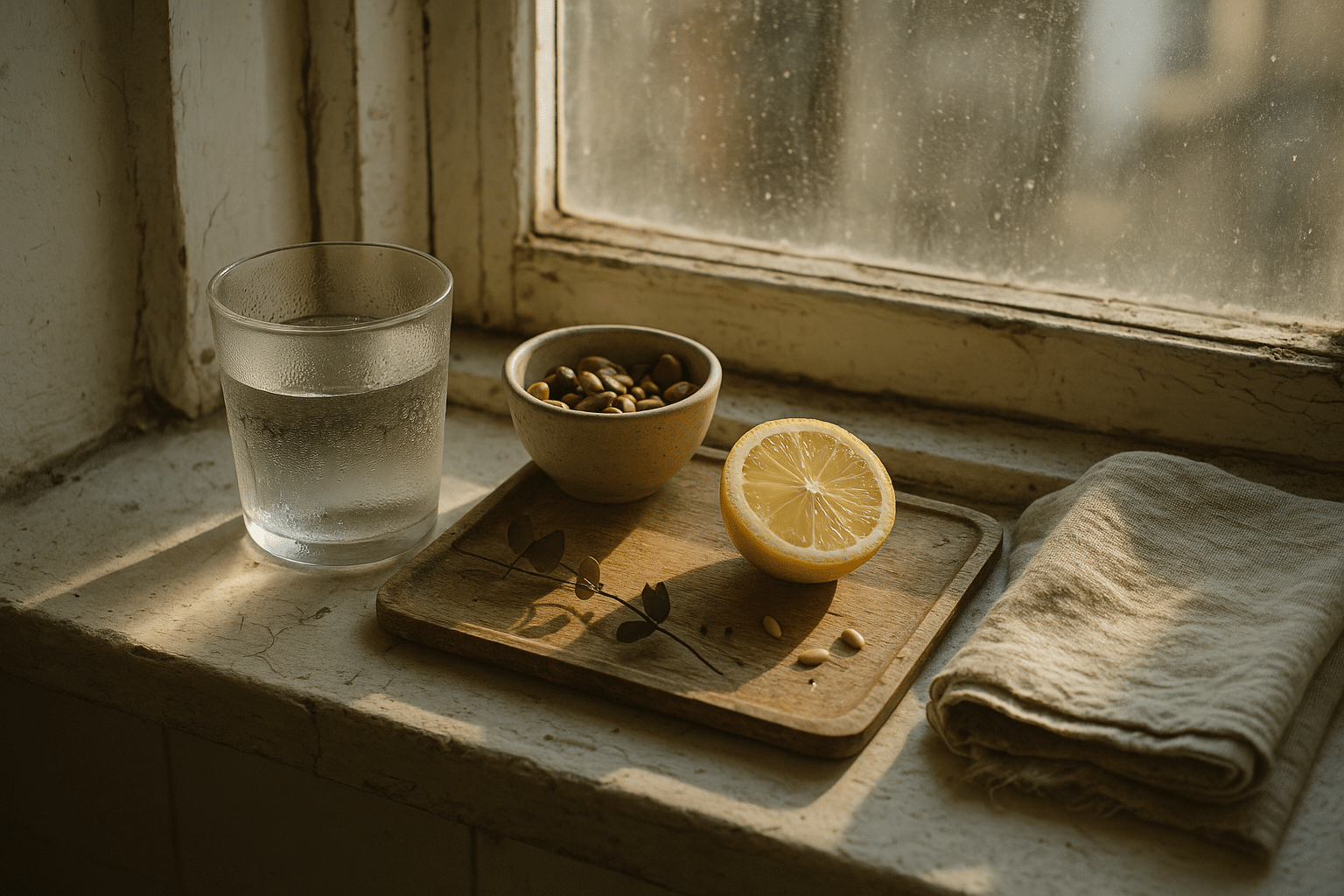
Temperature matters as much as timing. Unopened insulin is generally kept refrigerated—not frozen—while “in use” insulin is commonly stored at room temperature for a limited time as specified in official instructions. Heat, freezing, and direct sunlight can denature insulin, weakening its effect. Practical safeguards:
– Store backups in the main refrigerator compartment, not the door, to avoid temperature swings.
– Never freeze; if a vial or pen has been frozen or shows clumps, discoloration, or crystals, don’t use it.
– On hot days or during travel, use an insulated pouch with a cool—not ice‑cold—pack kept separate to avoid freezing.
Travel adds variables: time zones, meal timing shifts, and unpredictable temperatures. Pack more supplies than you think you need, split them between bags, and carry insulin with you rather than checking it where cargo holds can freeze. Keep a small thermometer in your kit if you travel frequently; it’s a simple way to validate that your storage plan is working. If you suspect compromised insulin—numbers trend higher despite proper dosing and technique—start a fresh pen or vial and monitor for improvement, then speak with your clinician about next steps. Thoughtful timing plus careful temperature control keeps the chemistry working in your favor.
Conclusion and Action Checklist
Getting insulin to perform consistently is part science, part routine. The science says absorption is shaped by tissue health, injection depth, and insulin structure, all of which respond to everyday choices. The routine piece is yours to own: small, repeatable steps that turn uncertainty into habits you can trust. If you’ve seen unexpected highs, tender spots, or frequent corrections, there’s a strong chance one of the three areas in this guide—rotation and needle reuse, injection technique, or timing and temperature—holds your next improvement.
Use this quick checklist to reinforce the essentials:
– I rotate sites methodically and avoid hardened or bruised areas.
– I use a new needle for each injection and discard it safely.
– I choose a needle length and angle that keep insulin in the subcutaneous layer, using a skinfold when needed.
– I prime my pen and, for cloudy types, mix until uniform before every dose.
– I press the plunger fully and hold for about 10 seconds before withdrawing.
– I match dose timing to my insulin’s action and the meal ahead, and I avoid stacking outside of my plan.
– I store insulin within recommended temperatures, avoiding heat, freezing, and direct sun.
What to expect when you put this into practice? Many people report fewer “mystery” highs, less discomfort, and a clearer pattern that makes dose adjustments—guided by your healthcare team—more straightforward. Improvements often show up within days as steadier curves on your meter or continuous monitor. If something still feels off after tightening your technique, bring detailed notes to your next appointment: where you injected, needle length, timing, and storage conditions. Those specifics give your clinician the clues needed to tailor your plan. You don’t have to overhaul everything at once; pick one change from the checklist, master it this week, and build from there. Consistency is quiet, but it’s powerful—dose by dose, day by day.