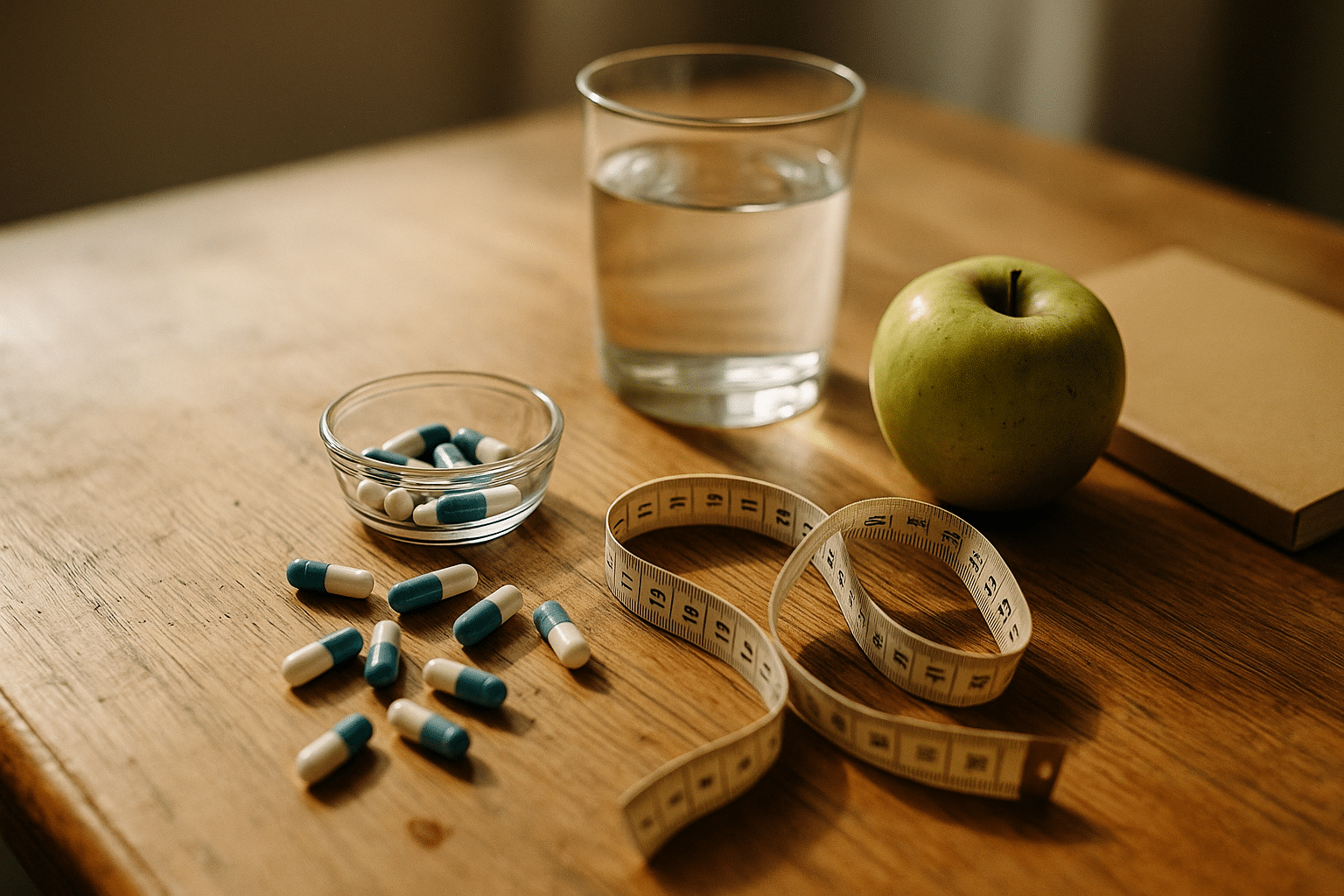
Weight Loss Pills That May Help: Evidence, Risks, and Safe Use
Why This Topic Matters, Plus a Quick Outline
Weight management affects health, daily energy, mobility, mental well-being, and long-term risk of conditions like type 2 diabetes and heart disease. Because of that, interest in weight loss pills keeps rising. Yet the marketplace mixes rigorous science with bold marketing, which can lead to confusion and disappointment. A practical approach is to understand which pills have credible evidence, what benefits are realistic, what risks exist, and how to use medications safely—if they are appropriate for you. Think of this article as a map: not a promise of shortcuts, but a way to navigate options without getting lost.
Before we dive deep, here is a brief outline of what follows:
– What counts as strong evidence for weight loss pills, and what average results look like
– A clear-eyed look at risks, side effects, and drug interactions you should know about
– A safety framework: who might qualify, what to monitor, and when to stop
– Practical comparisons to help you and your clinician choose a sensible option
It is important to define “weight loss pill.” In this guide, the term includes prescription oral medications designed or approved for long-term weight management, short-term appetite suppressants, and over-the-counter options (including supplements) sometimes used for weight control. Not every pill has equal evidence. Prescription agents typically have randomized controlled trials with hundreds to thousands of participants, whereas many supplements rely on small or lower-quality studies. Additionally, results are averages: individual responses vary based on genetics, habits, medical conditions, and adherence.
You will also see a recurring principle: medication is an adjunct to lifestyle, not a replacement. In studies, behavior changes—calorie awareness, fiber-forward eating, strength training, sleep routines—consistently magnify medication benefits and help keep weight off. Another theme is safety. Pills that act on appetite, absorption, or metabolism can interact with existing conditions and medications. For this reason, shared decision-making with a qualified clinician is essential. This article offers general education and does not substitute for personal medical advice.
Finally, expectations matter. Weight loss from pills is usually measured as percent of starting body weight over months, not days. The aim is clinically meaningful change—often a sustained 5–10% reduction—which can improve blood pressure, blood sugar, sleep apnea risk, joint pain, and liver health. With the outline in mind, let’s examine what the evidence actually shows.
What the Evidence Says: From Prescriptions to OTC
Evidence quality varies widely across weight loss pills. Randomized controlled trials (RCTs) and long-term follow-up data anchor the most reliable conclusions. Below is an overview of major categories, what mechanisms they use, and the results you might reasonably expect when these are combined with nutrition and activity guidance.
– Lipase inhibitor (orlistat): This medication reduces intestinal fat absorption by roughly a third when taken with meals containing fat. Across yearlong trials, average additional weight loss beyond placebo commonly lands near 3% of starting body weight, with a subset of users losing more. Some studies also reported improvements in cholesterol profiles and a reduced incidence of type 2 diabetes among higher-risk participants. Effectiveness depends heavily on dietary patterns; high-fat intake can trigger gastrointestinal side effects (discussed later), which indirectly encourages lower-fat choices.
– Sympathomimetic agents (e.g., phentermine) and combinations with an anticonvulsant (topiramate): Short-term use of single-agent appetite suppressants has yielded modest reductions—often about 3–5% over 12 weeks in responders. Longer-term data are stronger for the combination of phentermine with topiramate in extended-release form, where average total loss around a year can reach roughly 7–9% beyond lifestyle measures alone. Many participants achieve at least 5% loss, a threshold linked to metabolic benefits. However, tolerability and contraindications require careful screening.
– Opioid antagonist plus antidepressant (naltrexone with bupropion): By targeting reward pathways and appetite regulation, this combination has shown average losses of about 4–5% greater than placebo at one year, with nearly half of users achieving at least 5% loss when paired with a structured program. Nausea is common initially, and dose titration improves adherence.
– Incretin-based therapies taken orally (glucagon-like peptide-1 receptor agonists): While several agents in this class are injectables, oral forms have emerged and are being studied at higher doses specifically for obesity. Earlier, lower-dose oral formulations used for type 2 diabetes produced modest reductions, often in the range of 4–6% over many months, particularly when glucose control improved. More recent trials of higher-dose oral regimens have reported substantially larger average losses, reaching double-digit percentages over 1+ years. Availability, indications, and dosing vary by region, and ongoing studies continue to refine where these fit among oral options.
– Off-label and adjunctive options: Metformin, while not a weight loss drug, can yield small average reductions (often 2–3 kg) in some individuals, especially those with insulin resistance. Certain agents used for other indications may curb appetite or improve satiety as a secondary effect; however, they require individualized risk–benefit assessment and close follow-up.
– Over-the-counter products and supplements: Fiber-focused strategies (such as psyllium) may produce very modest losses via increased fullness and improved glycemic control, while improving digestive regularity. Caffeine and green tea extracts have shown small, short-term effects in some studies; the magnitude is often limited, and variability is high. Many herbal blends lack robust RCTs, and quality control can be inconsistent. A practical way to view OTC options: they may complement habits but rarely drive large, sustained changes on their own.
Translating numbers into expectations helps. If you start at 100 kg, a 5–10% reduction is 5–10 kg over several months. Trials usually pair medication with structured nutrition and activity, clinic visits, and supportive counseling—factors that meaningfully affect outcomes. Viewed this way, pills are tools that can amplify your efforts. The key is matching the tool to your medical history, preferences, access, and goals.
Risks, Side Effects, and Interactions You Should Know
All effective weight loss pills change physiology in ways that can carry trade-offs. Thinking in terms of “benefit versus risk” helps you make grounded choices. Below, you will find common side effects, red flags, and notable interactions for major categories.
– Lipase inhibitor (orlistat): Frequent gastrointestinal effects include oily spotting, urgency, flatulence with discharge, and steatorrhea, especially with high-fat meals. These effects usually improve when dietary fat is moderated. Rare but serious liver injury has been reported; seek evaluation for dark urine, jaundice, or right upper abdominal pain. Because fat absorption is reduced, fat-soluble vitamins (A, D, E, K) may drop; a multivitamin taken at a different time of day is often recommended.
– Sympathomimetics and the phentermine–topiramate combination: Elevated heart rate, increased blood pressure, insomnia, dry mouth, and anxiety can occur. People with significant cardiovascular disease, uncontrolled hypertension, hyperthyroidism, or a history of substance misuse may not be good candidates. Topiramate adds risks of paresthesia (tingling), altered taste, cognitive slowing (“word-finding” issues), and metabolic acidosis; it also increases the risk of birth defects, so reliable contraception and pregnancy testing are crucial for those who can become pregnant. Abrupt cessation of topiramate can provoke symptoms; dose changes should be supervised.
– Naltrexone with bupropion: Common issues include nausea, constipation, headache, and dizziness, especially during titration. Bupropion lowers seizure threshold; individuals with seizure disorders, eating disorders marked by purging, or heavy alcohol use require heightened caution or alternative therapies. This combination can raise blood pressure and heart rate; uncontrolled hypertension is a contraindication. Because naltrexone blocks opioid receptors, anyone using opioids for pain or opioid use disorder will experience reduced analgesia or precipitated withdrawal; a washout period and specialist involvement are essential.
– Oral incretin-based therapies: Nausea, vomiting, diarrhea, and early satiety are frequent at initiation and dose escalation but often improve over weeks. There are signals for increased risk of gallbladder disease and, rarely, pancreatitis; severe abdominal pain requires urgent assessment. Individuals with a history of medullary thyroid carcinoma or certain endocrine syndromes may be advised to avoid this class. Slower gastric emptying can alter absorption of oral medications; clinicians may adjust timing for drugs with narrow therapeutic windows.
Cross-cutting cautions apply to many agents: pregnancy and breastfeeding, adolescence, unmanaged eating disorders, and serious psychiatric conditions often warrant deferring pharmacotherapy or choosing alternatives with specialist input. Polypharmacy matters; for instance, combining stimulants with monoamine oxidase inhibitors is dangerous, and stacking multiple agents that raise blood pressure or heart rate increases risk. Alcohol use can complicate side effects and adherence. Liver and kidney function guide dosing and eligibility in several categories.
Practical safety steps include: baseline measurements (weight, waist, blood pressure, heart rate), relevant labs (metabolic panel, A1C if indicated, lipids), and medication reconciliation to catch interactions. Educate yourself on early side effects, as many are transient and manageable with dose titration and dietary tweaks. Watch for “red flag” symptoms—severe abdominal pain, chest pain, fainting, visual changes, or suicidal thoughts—and seek prompt care if they arise. Safety is not about worry; it is about being prepared.
Safe Use: Who Qualifies, What to Monitor, and When to Stop
There is a well-established framework for when to consider weight loss medication. Most guidelines suggest eligibility at body mass index (BMI) ≥30, or ≥27 with weight-related conditions such as type 2 diabetes, hypertension, dyslipidemia, obstructive sleep apnea, or osteoarthritis. Medication choice is individualized, balancing expected benefit, side effect profile, comorbidities, and patient preference. The goal is clinically meaningful improvement in health, not just a number on the scale.
Before starting, align on expectations and metrics. A common “response rule” is to assess progress after about 12 weeks on a therapeutic dose. If you have not lost at least 5% of starting weight by then—and if side effects are problematic—continuing that agent becomes less likely to help. This is not failure; it is feedback that guides a switch, a pause, or a new strategy. Conversely, responders often continue therapy longer, with periodic reviews to confirm ongoing benefit.
Monitoring keeps treatment safe and effective:
– Clinic checks: weight trend, waist circumference, blood pressure, heart rate, and side effect review
– Labs as indicated: A1C or fasting glucose, lipids, electrolytes, and liver or kidney tests for selected drugs
– Medication review: interactions, timing with meals, and adherence strategies (pillboxes, reminders)
– Lifestyle support: nutrition coaching, resistance training plan, sleep and stress routines
Side effect management is practical and often simple: ramp doses gradually, pair pills with food if advised, prioritize protein and fiber to tame appetite, and hydrate well. For gastric symptoms from incretin-based therapies, slower titration and smaller, more frequent meals help. For stimulant-related insomnia, avoid late dosing and discuss alternatives if sleep suffers. For lipase inhibition, trimming fried foods and emphasizing healthy fats in moderate amounts reduces urgency and bloating.
Stopping criteria matter. Consider pausing or discontinuing when any of these occur: sustained plateau below the 5% response threshold after an adequate trial, significant or persistent adverse effects, pregnancy planning, new contraindications, or patient preference. Some individuals transition to maintenance plans with lower doses or shift focus to non-pharmacologic tools. Weight regain is common after stopping—this reflects biology, not a lack of effort—so plan an “exit strategy” that includes continued food structure, activity, and follow-up.
Finally, document informed consent: what benefits you hope for, what risks you accept, and what milestones will trigger changes. Transparency and shared decision-making minimize surprises and turn a complex journey into a manageable, stepwise process.
Comparisons, Trade-offs, and Building a Realistic Plan
Choosing a weight loss pill is not about chasing headlines; it is about matching a tool to your health profile, budget, and preferences. Start by listing your priorities: appetite control, metabolic improvements, ease of use, side effect tolerance, or avoiding specific risks. Then consider the trade-offs across categories.
– If you have high blood pressure or arrhythmia risk, stimulant-based options may be less suitable; combinations that include an anticonvulsant or non-stimulant regimens might fit better.
– If you live with insulin resistance or fatty liver, agents that improve glycemic control and promote steady satiety can be appealing, provided you tolerate gastrointestinal effects and commit to gradual dose titration.
– If you experience gallbladder disease, discuss incretin-based therapies carefully and review warning signs.
– If you take chronic opioids, avoid antagonist-containing combinations to prevent withdrawal and loss of pain control.
– If you have a history of kidney stones, topiramate-containing regimens may require caution, increased hydration, or an alternative.
Access and cost considerations matter. Some agents have generic options with lower out-of-pocket expenses. Newer therapies can be highly effective but may involve higher monthly costs or prior authorization. Insurance coverage varies widely by region and indication, so verify benefits early. Adherence is more likely when your regimen is affordable, simple, and fits your daily rhythm—once-daily dosing, alignment with meals, and minimal side effects all help.
Pair your medication with habits that work in real life:
– Protein at most meals (roughly a palm or two), plenty of non-starchy vegetables, and high-fiber carbohydrates
– Resistance training two or three times weekly, plus regular walking or cycling for aerobic support
– A consistent sleep window and wind-down routine to stabilize appetite hormones
– Self-monitoring: a weekly weigh-in, a simple food log on busy weeks, and quarterly check-ins with your clinician or coach
Plan for plateaus. As weight drops, calorie needs fall, and progress slows. This is biology, not backsliding. Tactics include modest protein boosts, an extra day of resistance work, refining portion sizes, or brief periods of maintenance before resuming a gentle deficit. If you hit a sustained stall and have already optimized habits, revisit medication dose, timing, or class with your clinician.
Finally, define success broadly. A 7% loss with improved A1C, fewer joint flares, and better sleep may be more meaningful than a larger number that is hard to sustain. Map out milestones (first 5%, fitness goals, lab improvements), celebrations that are not food-centered, and a maintenance playbook. With thoughtful comparisons and a plan tailored to you, pills can serve as helpful companions—not captains—on your long-term health journey.
Conclusion: Turning Information into Action
Weight loss pills can help some people reach clinically meaningful goals, but they work best as part of a broader strategy anchored in nutrition, movement, sleep, and support. Evidence-backed options show average losses in the single to low double digits over many months, and the right match depends on your medical history, side effect tolerance, and access. A safety-first approach—eligibility screening, dose titration, response checks, and clear stop rules—protects your health while making steady progress more likely. Bring this framework to your next appointment, ask questions, and co-create a plan you can live with. With realistic expectations and consistent habits, you can translate information into durable change.